By Kara Clark and Ian Duncan
The E&R section sponsored a novel session at the Health Meeting in Atlanta in June. Titled, “Do you really use what you learn on exams?” the session aimed to address some of the topics that students are required to learn as part of their actuarial curriculum, but which they may not expect to ever have to use later in their actuarial careers. We picked three applications relevant to health actuaries to discuss: Credibility theory (in this case to the calibration of risk scores), Clinical subjects and Program Evaluation and the use of Markov Chains for modeling health care states.
Brad Armstrong, presenter of a talk on credibility has written an article that is published elsewhere in this edition of Expanding Horizons.
Brad was followed by Kara Clark, FSA, MAAA, senior director at Walgreens. She set the stage with my quote from the November/December 2014 issue of Contingencies : “… the health actuary of the future at a minimum will need to be part clinician, part behavioral psychologist, part health economist, and part epidemiologist.”
Kara’s presentation focused on applications in her work related to two books on the Group Health FSA syllabus: Managing and Evaluating Healthcare Intervention Programs, Second Edition, featured heavily on the Group & Health Advanced exam, and Healthcare Risk Adjustment and Predictive Modeling, (both published by Actex Publications) used on the Group & Health Specialty Exam.
With respect to the first book, Kara’s “real-world” examples included:
- Assessing the impact of pharmacist interventions on adherence;
- Analyzing utilization and cost of specific acute care episodes in retail clinics as compared to other sites of care;
- Evaluating financial and clinical outcomes produced by worksite health clinics;
- Designing and building client reporting on intervention programs;
- Modeling the impact of new treatment therapies and clinical interventions on the total cost of care;
- Defining and constructing “Clinical Quality Measures” based on data availability.
With respect to examples from the second book, Kara touched on:
- Conducting opportunity assessments of populations for management;
- Consulting on the build of predictive models;
- Using the results of predictive models to evaluate savings opportunities and estimate the return-on-investment for specific care intervention programs;
- Gaining familiarity with range of data sets (claims, clinical, activity, etc.) and the challenges of working with each.
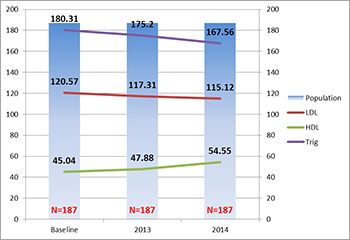
Kara gave a detailed example of designing reporting for a provider group interested in tracking clinical measures for a consistent chronic “patient panel” over time (that is, the provider group was interested in a consistent cohort rather than an ever-changing population). Not all encounter data was available for these patients; all that was available was encounter data for visits with the given provider group. This limitation meant that attribution to the patient panel could not be defined based on plurality of care, as is done with Accountable Care Organizations. In this case, when should a patient be considered part of the panel and when should a patient be excluded? If a patient is seen once a year for a chronic condition, is that sufficient to consider that patient part of the panel? Are two visits a year sufficient? Does each visit have to be related to the chronic condition (that is, if the patient was seen for a common cold, should that visit be excluded or included for purposes of determining whether the patient is part of the panel?) Should the criteria vary by condition? Similar questions had to be addressed relative to whether sufficient clinical data existed for each patient in the panel. If a patient was missing a lab value in one year, should the patient be excluded from the panel altogether? How would multiple lab values in a single year be addressed?
Illustrative Hyperlipidemia Patient Panel
In this example, principles from both books were used to wrestle through these definitions to ensure that the result aligned with the perspective of the clinicians on their practice as well as the practicalities of the available data.
Kara summarized her presentation with an observation that both books address different aspects of the care management value chain, including:
- Assessing and assembling the available data (whether claims, EHR, lab, activity, digital, self-reported, or other data);
- Conducting an opportunity assessment to identify pockets of members with less than optimal outcomes (whether financial or clinical) that we want to improve;
- Determining and designing the intervention;
- Building and validating predictive models to apply the intervention to the right members
- Operationalizing both the model and the intervention;
- Collecting data
- Assessing outcomes; and
- Providing a feedback loop for improving program design and operations.
Kara concluded by noting that the content knowledge she has gained from these two books has allowed her to communicate more effectively with other types of health care professionals that work along various aspects of this value chain, including (but not limited to) clinicians and health services researchers. In that way, she suggested that this syllabus content helps position actuaries for broader, more expansive roles in health care.
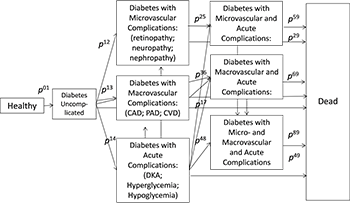
I finished up the session with a presentation of some research in which I am currently engaged, applying Semi-Markov models to health statuses. Markov-type models are in many ways ideally suited to modeling in health care because of the transitional nature of these statuses. I became interested in this topic through two routes. One, traditional predictive models often take a parametric approach to fitting models to claims data. These models can be quite successful and are the basis for much health actuarial work (Brad Armstrong’s article being an example of an application to risk adjustment). However, this modeling approach ignores what we know about underlying disease processes: the underlying pathway taken by different diseases. My hypothesis is that there is an underlying process, similar to a Markov process, at work, and that disease stages follow this process. An obvious example is diabetes, which progresses from pre-diabetes to diabetes, and then over time adds impairments to other systems (heart, kidneys, eyes, etc.). An example of a model of diabetes states is shown in Figure 1. P
Figure 1: Markov Model of Diabetes States
What is interesting from a modeling perspective is that the stages of chronic disease are often irreversible: while a disease can be managed, it can rarely be reversed. (A recent counter-example is Hepatitis C, which appears to be reversed by certain drugs, but this is an exception rather than the rule.) My second interest in the application of Markov models is because of the possibility of modeling the effect of interventions, such as drugs or programs on the underlying process. Let us assume that disease state progression is stable and can be estimated (i.e., the P
Health care does, however, have some features that make straightforward Markov models (as studied by students for the MLC exam) inappropriate. The most important of these is the statelessness of the Markov model, which means that the transition probability at a point depends only on the current state. In health care, we know that a patient’s current state is a function of prior states, and that the probability of transition depends on length of time in the current state—the probability of a patient to transition actually seems to follow (in some cases, anyway) a U-shaped distribution: those patients recently diagnosed and those diagnosed some time ago are more likely to transition.
This is a relatively new field for actuarial research and currently one in which researchers in the U.K. are leading. I hope that these examples will inspire students to see that what they learn for the exams is not dry mathematics, but has real application in their careers as actuaries.
Kara Clark, FSA, MAAA, is senior director Walgreens Clinical Outcomes & Analytics at Walgreens in Deerfield, Ill. She can be reached at kara.clark@walgreens.com.
Ian Duncan, FSA, FCA, FCIA, FIA, MAAA, is adjunct associate professor at University of California – Santa Barbara in Santa Barbara, Calif. He can be reached at duncan@pstat.ucsb.edu